How many people died from covid
How many people died from covid
Coronavirus (COVID-19) Mortality Rate
Last updated: May 14, 22:00 GMT
Introduction
When calculating the mortality rate, we need:
Considering that a large number of cases are asymptomatic (or present with very mild symptoms) and that testing has not been performed on the entire population, only a fraction of the SARS-CoV-2 infected population is detected, confirmed through a laboratory test, and officially reported as a COVID-19 case. The number of actual cases is therefore estimated to be at several multiples above the number of reported cases. The number of deaths also tends to be underestimated, as some patients are not hospitalized and not tested.
If we base our calculation (deaths / cases) on the number of reported cases (rather than on the actual ones), we will greatly overestimate the fatality rate.
Fatality Rate based on New York City Actual Cases and Deaths
Worldometer has analyzed the data provided by New York City, the New York State antibody study, and the excess deaths analysis by the CDC. Combining these 3 sources together we can derive the most accurate estimate to date on the mortality rate for COVID-19, as well as the mortality rate by age group and underlying condition. These findings can be valid for New York City and not necessarily for other places (suburban or rural areas, other countries, etc.), but they represent the best estimates to date given the co-occurrence of these 3 studies.
Actual Cases (1.7 million: 10 times the number of confirmed cases)
New York State conducted an antibody testing study [source], showing that 12.3% of the population in the state had COVID-19 antibodies as of May 1, 2020. The survey developed a baseline infection rate by testing 15,103 people at grocery stores and community centers across the state over the preceding two weeks. The study provides a breakdown by county, race (White 7%, Asian 11.1%, multi/none/other 14.4%, Black 17.4%, Latino/Hispanic 25.4%), and age, among other variables. 19.9% of the population of New York City had COVID-19 antibodies. With a population of 8,398,748 people in NYC [source], this percentage would indicate that 1,671,351 people had been infected with SARS-CoV-2 and had recovered as of May 1 in New York City. The number of confirmed cases reported as of May 1 by New York City was 166,883 [source], more than 10 times less.
Actual Deaths (23,000: almost twice the number of confirmed deaths)
As of May 1, New York City reported 13,156 confirmed deaths and 5,126 probable deaths (deaths with COVID-19 on the death certificate but no laboratory test performed), for a total of 18,282 deaths [source]. The CDC on May 11 released its «Preliminary Estimate of Excess Mortality During the COVID-19 Outbreak — New York City, March 11–May 2, 2020» [source] in which it calculated an estimate of actual COVID-19 deaths in NYC by analyzing the «excess deaths» (defined as «the number of deaths above expected seasonal baseline levels, regardless of the reported cause of death») and found that, in addition to the confirmed and probable deaths reported by the city, there were an estimated 5,293 more deaths to be attributed. After adjusting for the previous day (May 1), we get 5,148 additional deaths, for a total of actual deaths of 13,156 confirmed + 5,126 probable + 5,148 additional excess deaths calculated by CDC = 23,430 actual COVID-19 deaths as of May 1, 2020 in New York City.
Infection Fatality Rate (23k / 1.7M = 1.4% IFR)
Actual Cases with an outcome as of May 1 = estimated actual recovered (1,671,351) + estimated actual deaths (23,430) = 1,694,781.
Infection Fatality Rate (IFR) = Deaths / Cases = 23,430 / 1,694,781 = 1.4% (1.4% of people infected with SARS-CoV-2 have a fatal outcome, while 98.6% recover).
Mortality Rate (23k / 8.4M = 0.28% CMR to date) and Probability of Dying
As of May 1, 23,430 people are estimated to have died out of a total population of 8,398,748 in New York City. This corresponds to a 0.28% crude mortality rate to date, or 279 deaths per 100,000 population, or 1 death every 358 people. Note that the Crude Mortality Rate will continue to increase as more infections and deaths occur (see notes under the paragraph «Herd Immunity» below for details).
Mortality Rate by Age
When analyzing the breakdown of deaths by age and condition [source], we can observe how, out of 15,230 confirmed deaths in New York City up to May 12, only 690 (4.5% of all deaths) occurred in patients under the age of 65 who did not have an underlying medical condition (or for which it is unknown whether they had or did not have an underlying condition).
Underlying illnesses include Diabetes, Lung Disease, Cancer, Immunodeficiency, Heart Disease, Hypertension, Asthma, Kidney Disease, GI/Liver Disease, and Obesity [source]
Under 65-year-old (0.09% CMR to date)
85.9% of the population (7,214,525 people out of 8,398,748) in New York City is under 65 years old according to the US Census Bureau, which indicates the percent of persons 65 years old and over in New York City as being 14.1% [source].
We don’t know what percentage of the population in this age group has an underlying condition, so at this time we are not able to accurately estimate the fatality rate for the under 65 years old and healthy.
But we can calculate it for the entire population under 65 years old (both healthy and unhealthy): with 6,188 deaths (26% of the total deaths in all age groups) occurring in this age group, of which 5,498 deaths (89%) in patients with a known underlying condition, the crude mortality rate to date will correspond to 6,188 / 7,214,525 = 0.09% CMR, or 86 deaths per 100,000 population (compared to 0.28% and 279 deaths per 100,000 for the general population).
So far there has been 1 death every 1,166 people under 65 years old (compared to 1 death every 358 people in the general population). And 89% of the times, the person who died had one or more underlying medical conditions.
NOTE: We are gathering and analyzing additional data in order to provide more estimates by age group.
Herd Immunity and final Crude Mortality Rate
Crude mortality rate is not really applicable during an ongoing epidemic.
And to reach herd immunity for COVID-19 and effectively end the epidemic, approximately two thirds (67%) of the population would need to be infected. As of May 1, New York City is at 20%, based on the antibody study findings.
Therefore, the crude mortality rate has the potential to more than triple from our current estimate, reaching close to 1,000 deaths per 100,000 population (1% CMR), and close to 300 per 100,000 (0.3% CMR) in the population under 65 years old, with 89% of these deaths (267 out of 300) occurring in people with a known underlying medical condition (including obesity).
Historical Account of the Initial Estimates
3.4% Mortality Rate estimate by the World Health Organization (WHO) as of March 3
In his opening remarks at the March 3 media briefing on Covid-19, WHO Director-General Dr Tedros Adhanom Ghebreyesus stated:
“Globally, about 3.4% of reported COVID-19 cases have died. By comparison, seasonal flu generally kills far fewer than 1% of those infected.” [13]
Initial estimate was 2%
Initially, the World Health Organization (WHO) had mentioned 2% as a mortality rate estimate in a press conference on Wednesday, January 29 [1] [2] and again on February 10. However, on January 29 WHO specified that this was a very early and provisional estimate that might have changed. Surveillance was increasing, within China but also globally, but at the time it was said that:
Mortality Rate as of Feb. 20 in China (findings from the Report of the WHO-China Joint Mission)
The Report of the WHO-China Joint Mission published on Feb. 28 by WHO [12] is based on 55,924 laboratory confirmed cases. The report notes that «The Joint Mission acknowledges the known challenges and biases of reporting crude CFR early in an epidemic» (see also our discussion on: How to calculate the mortality rate during an outbreak). Here are its findings on Case Fatality Ratio, or CFR:
«As of 20 February, 2,114 of the 55,924 laboratory confirmed cases have died (crude fatality ratio [ CFR: 3.8% ) (note: at least some of whom were identified using a case definition that included pulmonary disease).
The overall CFR varies by location and intensity of transmission (i.e. 5.8% in Wuhan vs. 0.7% in other areas in China ).
In China, the overall CFR was higher in the early stages of the outbreak ( 17.3% for cases with symptom onset from 1-10 January) and has reduced over time to 0.7% for patients with symptom onset after 1 February. » [12]
Mortality Rate, as discussed by the National Health Commission (NHC) of China on Feb. 4
Asked at a press conference on February 4 what the current mortality rate (or case fatality rate, CFR) is, an official with China NHC said that [7] :
Preliminary study providing a tentative 3% estimate for case fatality rate
A preliminary study published on The Lancet on January 24 [3] provided an early estimation of 3% for the overall case fatality rate. Below we show an extract (highlights added for the relevant data and observations):
Of the 41 patients in this cohort, 22 (55%) developed severe dyspnoea and 13 (32%) required admission to an intensive care unit, and six died.
Hence, the case-fatality proportion in this cohort is approximately 14.6%, and the overall case fatality proportion appears to be closer to 3%.
However, both of these estimates should be treated with great caution because not all patients have concluded their illness (ie, recovered or died) and the true number of infections and full disease spectrum are unknown.
Importantly, in emerging viral infection outbreaks the case-fatality ratio is often overestimated in the early stages because case detection is highly biased towards the more severe cases.
As further data on the spectrum of mild or asymptomatic infection becomes available, one case of which was documented by Chan and colleagues, the case-fatality ratio is likely to decrease.
Nevertheless, the 1918 influenza pandemic is estimated to have had a case-fatality ratio of less than 5% but had an enormous impact due to widespread transmission, so there is no room for complacency.
Fatality rate can also change as a virus can mutate, according to epidemiologists.
Death rate among patients admitted to hospital
A study on 138 hospitalized patients with 2019-nCoV infection, published on February 7 on JAMA, found that 26% of patients required admission to the intensive care unit (ICU) and 4.3% died, but a number of patients were still hospitalized at the time. [9]
A previous study had found that, out of 41 admitted hospital patients, 13 (32%) patients were admitted to an ICU and six (15%) died. [5]
Days from first symptom to death
The Wang et al. February 7 study published on JAMA found that the median time from first symptom to dyspnea was 5.0 days, to hospital admission was 7.0 days, and to ARDS was 8.0 days. [9]
Previously. the China National Health Commission reported the details of the first 17 deaths up to 24 pm 22 Jan 2020. A study of these cases found that the median days from first symptom to death were 14 (range 6-41) days, and tended to be shorter among people of 70 year old or above (11.5 [range 6-19] days) than those with ages below 70 year old (20 [range 10-41] days. [6]
Median Hospital Stay
The JANA study found that, among those discharged alive, the median hospital stay was 10 days. [9]
Comparison with other viruses
For comparison, the case fatality rate with seasonal flu in the United States is less than 0.1% (1 death per every 1,000 cases).
Mortality rate for SARS was 10%, and for MERS 34%.
How to calculate the mortality rate during an outbreak
At present, it is tempting to estimate the case fatality rate by dividing the number of known deaths by the number of confirmed cases. The resulting number, however, does not represent the true case fatality rate and might be off by orders of magnitude [. ]
A precise estimate of the case fatality rate is therefore impossible at present.
The case fatality rate (CFR) represents the proportion of cases who eventually die from a disease.
Once an epidemic has ended, it is calculated with the formula: deaths / cases.
But while an epidemic is still ongoing, as it is the case with the current novel coronavirus outbreak, this formula is, at the very least, «naïve» and can be «misleading if, at the time of analysis, the outcome is unknown for a non negligible proportion of patients.» [8]
In other words, current deaths belong to a total case figure of the past, not to the current case figure in which the outcome (recovery or death) of a proportion (the most recent cases) hasn’t yet been determined.
The correct formula, therefore, would appear to be:
CFR = deaths at day.x / cases at day.x-
This would constitute a fair attempt to use values for cases and deaths belonging to the same group of patients.
One issue can be that of determining whether there is enough data to estimate T with any precision, but it is certainly not T = 0 (what is implicitly used when applying the formula current deaths / current cases to determine CFR during an ongoing outbreak).
Let’s take, for example, the data at the end of February 8, 2020: 813 deaths (cumulative total) and 37,552 cases (cumulative total) worldwide.
If we use the formula (deaths / cases) we get:
813 / 37,552 = 2.2% CFR (flawed formula).
With a conservative estimate of T = 7 days as the average period from case confirmation to death, we would correct the above formula by using February 1 cumulative cases, which were 14,381, in the denominator:
Feb. 8 deaths / Feb. 1 cases = 813 / 14,381 = 5.7% CFR (correct formula, and estimating T=7).
T could be estimated by simply looking at the value of (current total deaths + current total recovered) and pair it with a case total in the past that has the same value. For the above formula, the matching dates would be January 26/27, providing an estimate for T of 12 to 13 days. This method of estimating T uses the same logic of the following method, and therefore will yield the same result.
An alternative method, which has the advantage of not having to estimate a variable, and that is mentioned in the American Journal of Epidemiology study cited previously as a simple method that nevertheless could work reasonably well if the hazards of death and recovery at any time t measured from admission to the hospital, conditional on an event occurring at time t, are proportional, would be to use the formula:
CFR = deaths / (deaths + recovered)
which, with the latest data available, would be equal to:
6,454,202 / (6,454,202 + 544,907,396) = 1% CFR (worldwide)
If we now exclude cases in mainland China, using current data on deaths and recovered cases, we get:
6,448,976 / (6,448,976 + 544,682,953) = 1.2% CFR (outside of mainland China)
The sample size above is limited, and the data could be inaccurate (for example, the number of recoveries in countries outside of China could be lagging in our collection of data from numerous sources, whereas the number of cases and deaths is more readily available and therefore generally more up to par).
There was a discrepancy in mortality rates (with a much higher mortality rate in China) which however is not being confirmed as the sample of cases outside of China is growing in size. On the contrary, it is now higher outside of China than within.
That initial discrepancy was generally explained with a higher case detection rate outside of China especially with respect to Wuhan, where priority had to be initially placed on severe and critical cases, given the ongoing emergency.
Unreported cases would have the effect of decreasing the denominator and inflating the CFR above its real value. For example, assuming 10,000 total unreported cases in Wuhan and adding them back to the formula, we would get a CFR of 1.2% (quite different from the CFR of 1% based strictly on confirmed cases).
Neil Ferguson, a public health expert at Imperial College in the UK, said his “best guess” was that there were 100,000 affected by the virus even though there were only 2,000 confirmed cases at the time. [11]
Without going that far, the possibility of a non negligible number of unreported cases in the initial stages of the crisis should be taken into account when trying to calculate the case fatally rate.
As the days go by and the city organized its efforts and built the infrastructure, the ability to detect and confirm cases improved. As of February 3, for example, the novel coronavirus nucleic acid testing capability of Wuhan had increased to 4,196 samples per day from an initial 200 samples. [10]
A significant discrepancy in case mortality rate can also be observed when comparing mortality rates as calculated and reported by China NHC: a CFR of 3.1% in the Hubei province (where Wuhan, with the vast majority of deaths is situated), and a CFR of 0.16% in other provinces (19 times less).
Finally, we shall remember that while the 2003 SARS epidemic was still ongoing, the World Health Organization (WHO) reported a fatality rate of 4% (or as low as 3%), whereas the final case fatality rate ended up being 9.6%.
Coronavirus (COVID-19) Cases
We are grateful to everyone whose editorial review and expert feedback on this work helps us to continuously improve our work on the pandemic. Thank you. Here you find the acknowledgements.
The data on the coronavirus pandemic is updated daily.
Our work belongs to everyone
Explore the global data on confirmed COVID-19 cases
Select countries to show in all charts
This page has a large number of charts on the pandemic. In the box below you can select any country you are interested in – or several, if you want to compare countries.
All charts on this page will then show data for the countries that you selected.
Confirmed cases
What is the daily number of confirmed cases?
Related charts:
Which world regions have the most daily confirmed cases?
This chart shows the number of confirmed COVID-19 cases per day.
What is important to note about these case figures?
→ We provide more detail on these points in the section ‘Cases of COVID-19: background‘.
Five quick reminders on how to interact with this chart
Daily confirmed cases per million people
Differences in the population size between different countries are often large – it is insightful to compare the number of confirmed cases per million people.
Keep in mind that in countries that do very little testing the actual number of cases can be much higher than the number of confirmed cases shown here.
Three tips on how to interact with this map
What is the cumulative number of confirmed cases?
Related charts:
Which world regions have the most cumulative confirmed cases?
How do the number of tests compare to the number of confirmed COVID-19 cases? See them plotted against each other.
The previous charts looked at the number of confirmed cases per day – this chart shows the cumulative number of confirmed cases since the beginning of the COVID-19 pandemic.
Cumulative confirmed cases per million people
This chart shows the cumulative number of confirmed cases per million people.
Weekly and biweekly cases: where are confirmed cases increasing or falling?
Why is it useful to look at weekly or biweekly changes in confirmed cases?
For all global data sources on the pandemic, daily data does not necessarily refer to the number of new confirmed cases on that day – but to the cases reported on that day.
Since reporting can vary significantly from day to day – irrespectively of any actual variation of cases – it is helpful to look at changes from week to week. This provides a slightly clearer picture of where the pandemic is accelerating, slowing, or in fact reducing.
The maps shown here provide figures on weekly and biweekly confirmed cases: one set shows the number of confirmed cases per million people in the previous seven (or fourteen) days (the weekly or biweekly cumulative total); the other set shows the percentage change (growth rate) over these periods.
Click to open interactive version
Click to open interactive version
Click to open interactive version
Click to open interactive version
Global comparison: where are confirmed cases increasing most rapidly?
Simply looking at the cumulative total or daily number of confirmed cases does not allow us to understand or compare the speed at which these figures are rising.
The table here shows how long it has taken for the number of confirmed cases to double in each country for which we have data. The table also shows both the cumulative total and daily new number of confirmed cases, and how those numbers have changed over the last 14 days.
How you can interact with this table
You can sort the table by any of the columns by clicking on the column header.
Coronavirus sequences by variant
About this data
Our data on SARS-CoV-2 sequencing and variants is sourced from GISAID, a global science initiative that provides open-access to genomic data of SARS-CoV-2. We recognize the work of the authors and laboratories responsible for producing this data and sharing it via the GISAID initiative.
Khare, S., et al (2021) GISAID’s Role in Pandemic Response. China CDC Weekly, 3(49): 1049-1051. doi: 10.46234/ccdcw2021.255 PMCID: 8668406
Elbe, S. and Buckland-Merrett, G. (2017) Data, disease and diplomacy: GISAID’s innovative contribution to global health. Global Challenges, 1:33-46. doi:10.1002/gch2.1018 PMCID: 31565258
Shu, Y. and McCauley, J. (2017) GISAID: from vision to reality. EuroSurveillance, 22(13) doi:10.2807/1560-7917.ES.2017.22.13.30494 PMCID: PMC5388101
We download aggregate-level data via CoVariants.org.
All countries report data on the results from sequenced samples every 14 days, although some of them may share partial data in advance. We obtain the share of each variant by dividing the number of sequences labelled for that variant by the total number of sequences. Since only a fraction of all cases are sequenced, this share may not reflect the complete breakdown of cases. In addition, recently-discovered or actively-monitored variants may be overrepresented, as suspected cases of these variants are likely to be sequenced preferentially or faster than other cases.
Click to open interactive version
Click to open interactive version
Click to open interactive version
Confirmed deaths and cases: our data source
Our World in Data relies on data from Johns Hopkins University
The Johns Hopkins University dashboard and dataset is maintained by a team at its Center for Systems Science and Engineering (CSSE). It has been publishing updates on confirmed cases and deaths for all countries since January 22, 2020. A feature on the JHU dashboard and dataset was published in The Lancet in early May 2020. 1 This has allowed millions of people across the world to track the course and evolution of the pandemic.
JHU updates its data multiple times each day. This data is sourced from governments, national and subnational agencies across the world — a full list of data sources for each country is published on Johns Hopkins’s GitHub site. It also makes its data publicly available there.
Cases of COVID-19: background
How is a COVID-19 case defined?
In epidemiology, individuals who meet the case definition of a disease are often categorized on three different levels.
These definitions are often specific to the particular disease, but generally have some clear and overlapping criteria.
Cases of COVID-19 – as with other diseases – are broadly defined under a three-level system: suspected, probable and confirmed cases.
Typically, for a case to be confirmed, a person must have a positive result from laboratory tests. This is true regardless of whether they have shown symptoms of COVID-19 or not.
This means that the number of confirmed cases is lower than the number of probable cases, which is in turn lower than the number of suspected cases. The gap between these figures is partially explained by limited testing for the disease.
How are cases reported?
We have three levels of case definition: suspected, probable and confirmed cases. What is measured and reported by governments and international organizations?
International organizations – namely the WHO and European CDC – report case figures submitted by national governments. Wherever possible they aim to report confirmed cases, for two key reasons:
1. They have a higher degree of certainty because they have laboratory confirmation;
2. They help to provide standardised comparisons between countries.
However, international bodies can only provide figures as submitted by national governments and reporting institutions. Countries can define slightly different criteria for how cases are defined and reported. 4 Some countries have, over the course of the outbreak, changed their reporting methodologies to also include probable cases.
One example of this is the United States. Until 14 th April 2020 the US CDC provided daily reports on the number of confirmed cases. However, as of 14 th April, it now provides a single figure of cases: the sum of confirmed and probable cases.
Suspected case figures are usually not reported. The European CDC notes that suspected cases should not be reported at the European level (although countries may record this information for national records) but are used to understand who should be tested for the disease.
Reported new cases on a particular day do not necessarily represent new cases on that day
The number of confirmed cases reported by any institution – including the WHO, the ECDC, Johns Hopkins and others – on a given day does not represent the actual number of new cases on that date. This is because of the long reporting chain that exists between a new case and its inclusion in national or international statistics.
The steps in this chain are different across countries, but for many countries the reporting chain includes most of the following steps:
This reporting chain can take several days. This is why the figures reported on any given date do not necessarily reflect the number of new cases on that specific date.
The number of actual cases is higher than the number of confirmed cases
To understand the scale of the COVID-19 outbreak, and respond appropriately, we would want to know how many people are infected by COVID-19. We would want to know the actual number of cases.
However, the actual number of COVID-19 cases is not known. When media outlets claim to report the ‘number of cases’ they are not being precise and omit to say that it is the number of confirmed cases they speak about.
The actual number of cases is not known, not by us at Our World in Data, nor by any other research, governmental or reporting institution.
The number of confirmed cases is lower than the number of actual cases because not everyone is tested. Not all cases have a “laboratory confirmation”; testing is what makes the difference between the number of confirmed and actual cases.
All countries have been struggling to test a large number of cases, which means that not every person that should have been tested has been tested.
Since an understanding of testing for COVID-19 is crucial for an interpretation of the reported numbers of confirmed cases we have looked into the testing for COVID-19 in more detail.
You find our work on testing here. In a separate post we discuss how models of COVID-19 help us estimate the actual number of cases.
Acknowledgements
We would like to acknowledge and thank a number of people in the development of this work: Carl Bergstrom, Bernadeta Dadonaite, Natalie Dean, Joel Hellewell, Jason Hendry, Adam Kucharski, Moritz Kraemer and Eric Topol for their very helpful and detailed comments and suggestions on earlier versions of this work. We thank Tom Chivers for his editorial review and feedback.
And we would like to thank the many hundreds of readers who give us feedback on this work. Your feedback is what allows us to continuously clarify and improve it. We very much appreciate you taking the time to write. We cannot respond to every message we receive, but we do read all feedback and aim to take the many helpful ideas into account.
Endnotes
The European CDC discusses the criteria for what constitutes a probable case, and a ‘close contact’ here.
See any Situation Report by the WHO – for example Situation Report 50.
The WHO also speaks of ‘suspected cases’ and ‘probable cases’, but the WHO Situation Reports do not provide figures on ‘probable cases’, and only report ‘suspected cases’ for Chinese provinces (‘suspected cases’ by country is not available).
In Situation Report 50 they define these as follows:
Suspect case
A. A patient with acute respiratory illness (fever and at least one sign/symptom of respiratory disease (e.g., cough, shortness of breath), AND with no other etiology that fully explains the clinical presentation AND a history of travel to or residence in a country/area or territory reporting local transmission (See situation report) of COVID-19 disease during the 14 days prior to symptom onset.
OR
B. A patient with any acute respiratory illness AND having been in contact with a confirmed or probable COVID19 case (see definition of contact) in the last 14 days prior to onset of symptoms;
OR
C. A patient with severe acute respiratory infection (fever and at least one sign/symptom of respiratory disease (e.g., cough, shortness breath) AND requiring hospitalization AND with no other etiology that fully explains the clinical presentation.
Probable case
A suspect case for whom testing for COVID-19 is inconclusive. Inconclusive being the result of the test reported by the laboratory.
The US, for example, uses the following definitions: “A confirmed case or death is defined by meeting confirmatory laboratory evidence for COVID-19. A probable case or death is defined by i) meeting clinical criteria AND epidemiologic evidence with no confirmatory laboratory testing performed for COVID-19; or ii) meeting presumptive laboratory evidence AND either clinical criteria OR epidemiologic evidence; or iii) meeting vital records criteria with no confirmatory laboratory testing performed for COVID19.”
Reuse our work freely
All visualizations, data, and code produced by Our World in Data are completely open access under the Creative Commons BY license. You have the permission to use, distribute, and reproduce these in any medium, provided the source and authors are credited.
The data produced by third parties and made available by Our World in Data is subject to the license terms from the original third-party authors. We will always indicate the original source of the data in our documentation, so you should always check the license of any such third-party data before use and redistribution.
Citation
Our articles and data visualizations rely on work from many different people and organizations. When citing this entry, please also cite the underlying data sources. This entry can be cited as:
How do death rates from COVID-19 differ between people who are vaccinated and those who are not?
To understand how the pandemic is evolving, it’s crucial to know how death rates from COVID-19 are affected by vaccination status. The death rate is a key metric that can accurately show us how effective vaccines are against severe forms of the disease. This may change over time when there are changes in the prevalence of COVID-19, and because of factors such as waning immunity, new strains of the virus, and the use of boosters.
On this page, we explain why it is essential to look at death rates by vaccination status rather than the absolute number of deaths among vaccinated and unvaccinated people.
We also visualize this mortality data for the United States, England, Switzerland, and Chile.
Ideally we would produce a global dataset that compiles this data for countries around the world, but we do not have the capacity to do this in our team. As a minimum, we list country-specific sources where you can find similar data for other countries, and we describe how an ideal dataset would be formatted.
Why we need to compare the rates of death between vaccinated and unvaccinated
During a pandemic, you might see headlines like “Half of those who died from the virus were vaccinated”.
It would be wrong to draw any conclusions about whether the vaccines are protecting people from the virus based on this headline. The headline is not providing enough information to draw any conclusions.
Let’s think through an example to see this.
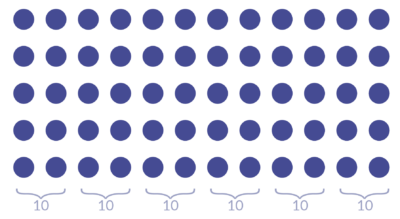
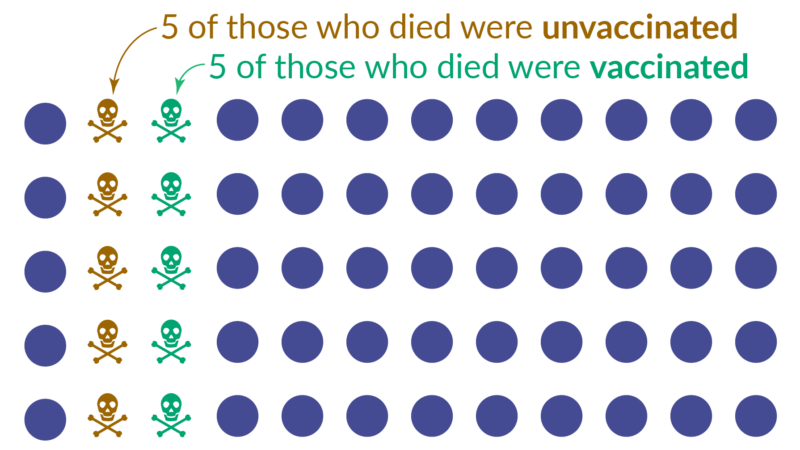
Imagine we live in a place with a population of 60 people.
Then we learn that 10 people died. And we learn that 50% of them were vaccinated.
The newspaper may run the headline “Half of those who died from the virus were vaccinated”. But this headline does not tell us anything about whether the vaccine is protecting people or not.
To be able to say anything, we also need to know about those who did not die: how many people in this population were vaccinated? And how many were not vaccinated?
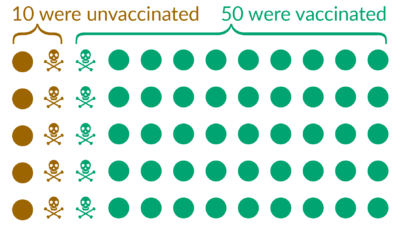
Now we have all the information we need and can calculate the death rates:
We therefore see that the death rate among the vaccinated is 5-times lower than among the unvaccinated.
In the example, we invented numbers to make it simple to calculate the death rates. But the same logic applies also in the current COVID-19 pandemic. Comparisons of the absolute numbers, as some headlines do, is making a mistake that’s known in statistics as a ‘base rate fallacy’: it ignores the fact that one group is much larger than the other. It is important to avoid this mistake, especially now, as in more and more countries the number of people who are vaccinated against COVID-19 is much larger than the number of people who are unvaccinated (see our vaccination data).
This example was illustrating how to think about these statistics in a hypothetical case. Below, you can find the real data for the situation in the COVID-19 pandemic now.
Data on COVID-19 mortality by vaccination status
Here we bring together the official mortality data by vaccination status published by the United States, England, Switzerland, and Chile. These charts are updated weekly, if new data has been published by the official source.
Switzerland
Switzerland has fully vaccinated 69.1% of its population, mostly with the mRNA vaccines produced by Pfizer and Moderna. Mortality data by vaccination status is published by the Federal Office of Public Health (data coverage also includes Liechtenstein).
This chart presents the COVID-19 death rate among unvaccinated people, among fully-vaccinated people, and among those who additionally received a booster dose.
You can click the “Change age group” button on the top left to explore data for a specific age group.
The mortality rate for the “All ages” group is age-standardized by Our World in Data, using single-year age estimates from the 2022 revision of the United Nations World Population Prospects for Switzerland. Rates for specific age groups are calculated as crude incidence rates.
Click to open interactive version
United States
The United States has fully vaccinated 67.3% of its population, mostly with the mRNA vaccines produced by Pfizer and Moderna. Mortality data by vaccination status is published by the US CDC.
This chart presents the COVID-19 death rate among unvaccinated people (0 doses received), people with a full primary vaccination series, those who received 1 booster dose, and those who received 2 booster doses.
You can click the “Change age group” button on the top left to explore data for a specific age group.
The mortality rate for the “All ages” group is age-standardized by the US CDC using the 2000 US Census standard population. Rates for specific age groups are calculated as crude incidence rates.
Click to open interactive version
Chile
Chile has fully vaccinated 90.5% of its population, mostly with the Sinovac vaccine. Mortality data by vaccination status is published by the Ministry of Health.
This chart presents the COVID-19 death rate among people who are not fully vaccinated, among fully-vaccinated people, and among those who additionally received a booster dose.
You can click the “Change age group” button on the top left to explore data for a specific age group.
The mortality rate for the “All ages” group is age-standardized by Our World in Data, using single-year age estimates from the 2022 revision of the United Nations World Population Prospects for Chile. Rates for specific age groups are calculated as crude incidence rates.
The pandemic’s true death toll
Our daily estimate of excess deaths around the world
H ow many people have died because of the covid-19 pandemic? The answer depends both on the data available, and on how you define “because”. Many people who die while infected with SARS-CoV-2 are never tested for it, and do not enter the official totals. Conversely, some people whose deaths have been attributed to covid-19 had other ailments that might have ended their lives on a similar timeframe anyway. And what about people who died of preventable causes during the pandemic, because hospitals full of covid-19 patients could not treat them? If such cases count, they must be offset by deaths that did not occur but would have in normal times, such as those caused by flu or air pollution.
The reason that we can provide only a rough estimate, with a wide range of surrounding uncertainty, is that calculating excess deaths for the entire world is complex and imprecise. Including statistics released by sub-national units like provinces or cities, among the world’s 156 countries with at least 1m people we managed to obtain data on total mortality from just 84. Some of these places update their figures regularly; others have published them only once.
To fill in these voids in our understanding of the pandemic, The Economist has built a machine-learning model, which estimates excess deaths for every country on every day since the pandemic began. It is based both on official excess-mortality data and on more than 100 other statistical indicators. Our final tallies use governments’ official excess-death numbers whenever and wherever they are available, and the model’s estimates in all other cases. You can read our methodology here, and inspect all our code, data, and models here.
In the chart above, you can explore our numbers either for the world as a whole or broken down by region. Our model provides a range (the coloured interval) and a central estimate (the line). The less data that are available in a given country, the less certain we can be about how many excess deaths have actually occurred there, and thus the wider our confidence interval becomes. The most recent cumulative totals are also available below, in table format.
The regional estimates above are aggregations of our figures for individual countries. Differences between countries in the scale and frequency of testing for SARS-CoV-2—which, along with the severity of the pandemic, determine the official covid-19 death toll—can be vast. Excess-deaths data are essential in order to make comparisons between countries on an apples-to-apples basis. In cases where death rates fell below their pre-pandemic norms—because covid-19 claimed relatively few victims, while lifestyle changes lowered the toll from other causes such as flu—this number is negative.
The interactive chart above lets you compare excess mortality over time in any pair of countries. You can also look up the cumulative total for individual countries in the subsequent table. Although we provide an estimated excess-deaths figure for every day since the pandemic began, official covid-19 death statistics are displayed only up to the most recent data release, and are missing afterwards.
These data make clear that covid-19 has led to the deaths of far more people than official statistics suggest (see our briefing). Measured by excess deaths as a share of population, many of the world’s hardest-hit countries are in Latin America. Although Russia’s official death tally suggests that it has protected its citizens tolerably well, its numbers on total mortality imply that it has in fact been hit quite hard by covid-19. Similarly, we estimate that India’s death toll is actually in the millions, rather than the hundreds of thousands. At the other end of the table, a handful of countries have actually had fewer people die during the pandemic than in previous years.
Although excess-deaths statistics are the most comprehensive measure of the human cost of covid-19, they are only loosely tied to the number of people who have been infected with SARS-CoV-2. Because the virus is so much deadlier for older people than it is among the young, death tolls are heavily influenced by the age structure of a country’s population. Holding other factors constant, it takes a smaller number of infections to produce a given number of excess deaths in places where lots of people are aged over 65 than in those where relatively few people are vulnerable. As a result, excess-death data can only be used as a good indicator of the spread of covid-19 if you also account for demography.
The two maps above display some of the implications of this relationship. The first shows excess deaths as a share of each country’s population aged at least 65, a very simple guide to how widely covid-19 is likely to have spread. The second depicts an estimate of the share of people in each country who have been infected. To calculate it, we divide a country’s total excess deaths by a context-adjusted infection-fatality risk: the chance that a person selected from the country’s population at random would die after catching covid-19, assuming medical treatment at rich-world standards. The younger a country’s population is, the lower this probability becomes.
This estimate is extremely rough. It accounts neither for variation between countries in the propensity of members of particular demographic groups to get infected, nor for differences in the prevalence of underlying medical conditions that increase vulnerability to covid-19. Because good medical treatment is harder to come by in poor countries, it overestimates the number of cases in such places. In some countries, this yields an estimate of total infections that exceeds a country’s population—a scenario that is theoretically possible, since reinfections do occur, but is probably quite unlikely.
This method also does not incorporate data on vaccinations, which have sharply lowered the infection-fatality rate in 2021 in many countries. And it lacks information about the prevalence of new variants of SARS-CoV-2 such as Alpha and Delta, which may have a different degree of virulence from the original strain. Despite all of these caveats, this approach at least provides a starting point for estimating how many people have caught the virus that does not depend on the vagaries of testing programmes. You can explore both of these sets of numbers for each country in the table below.
There are two main ways that our excess-death tallies could misrepresent reality. The first is that they rely on the assumption that officially published excess-mortality numbers are accurate. Given the disruption that covid-19 has caused, it is plausible that some governments may have changed how they compile data on total deaths during the pandemic. This might lead us to publish incorrect figures for the countries in question. It could also introduce errors into the estimates that our model produces for all other countries.
Second, because most countries that report excess deaths are rich or middle-income, the bulk of the data used to train our model comes from such places. The patterns that the model detects in these areas could thus be an inaccurate guide to the dynamics of the pandemic in poor countries. A similar caveat applies to our estimates for countries that have suffered lots of excess deaths for reasons other than the pandemic, such as war or natural disasters.
Our excess-deaths tally will be updated every day on this page. We hope readers return to it regularly to enrich their understanding of the path of the pandemic, around the world and over time. We will also continue trying to improve our model. Below, you can see a record of all the changes we have made to it so far. ■
Non-reporting countries
Turkmenistan has not reported any covid-19 figures since the start of the pandemic. It also has not published all-cause mortality data. Estimates for this country are therefore especially uncertain.
Model changelog
Read our methodology here, and inspect all our code, data, and models on GitHub.
Feb 7th 2022
Sep 2nd 2021
Sources
Excess deaths: The Economist; Human Mortality Database; World Mortality Dataset; Registro Civil (Bolivia); Vital Strategies; Office for National Statistics; Northern Ireland Statistics and Research Agency; National Records of Scotland; Registro Civil (Chile); Registro Civil (Ecuador); Institut National de la Statistique et des Études Économiques; Santé Publique France; Istituto Nazionale di Statistica; Dipartimento della Protezione Civile; Secretaría de Salud (Mexico); Ministerio de Salud (Peru); Data Science Research Peru; Departamento Administrativo Nacional de Estadística (Colombia); South African Medical Research Council; Instituto de Salud Carlos III; Ministerio de Sanidad (Spain); Datadista; Liu et al (2021)
Excess deaths (subnational): Local Mortality Dataset; Rukmini S (2021); Sumitra Debroy (2021); Thejesh GN (2021); Srinivasan Ramani and Vignesh Radhakrishnan (2021); Jakarta Open Data
Covid-19 data (deaths, cases, testing, and vaccinations): Our World In Data; Johns Hopkins University, CSSE; Covid19India.org; Jakarta covid-19 response team
Prevalence of covid-19 antibodies: SeroTracker.com
Demography and urbanization rates: Our World in Data; World Bank; United Nations; World Health Organization; World Population Review
Demography-adjusted infection fatality rate: The Economist, based on Brazeau et al. (2020) and UN population figures
Health outcomes and healthcare quality: Our World in Data; World Bank; WHO
Political regime and media freedom data: V-Dem Institute; PolityIV Project; Freedom House; Boix et al (2015)
Economy and connectivity: World Bank; Our World in Data; World Tourism Organization
Mobility: COVID-19 Community Mobility Reports (Google)
Geography: Natural Earth; Decker et al (“maps” R package); Mayer T et al (2011); Gallup et al (2010)
Government policy responses to Covid-19: OxCGRT (University of Oxford)
Mortality Risk of COVID-19
We are grateful to everyone whose editorial review and expert feedback on this work helps us to continuously improve our work on the pandemic. Thank you. Here you find the acknowledgements.
The data on the coronavirus pandemic is updated daily.
Our interactive data visualizations that show the case fatality rate in each country are updated daily.
The text below is updated periodically. In the last update we replaced some of the earlier content on mortality risks by age and preexisting health conditions from before vaccines were available.
Case fatality rate
Related chart:
How do the total number of confirmed deaths and cases compare? See them plotted against each other.
How has the number of confirmed cases and confirmed deaths changed over time?
The case fatality rate (CFR) is simply the number of confirmed deaths divided by the number of confirmed cases.
This chart here plots the CFR calculated in this way.
When the number of actual cases and deaths is not known – as is the case for COVID – one has to be careful in interpreting the CFR. In the sections that follow we explain what we can and cannot learn about the mortality risk based on the CFR.
Understanding the case fatality, crude mortality, and the infection fatality rate
Case fatality rate (CFR)
In the media, it is often the “case fatality rate” that is talked about when the risk of death from COVID-19 is discussed. 1
This measure is sometimes also called case fatality risk or case fatality ratio. It is often abbreviated as CFR.
The CFR is not the same as the risk of death for an infected person – even though, unfortunately, journalists sometimes suggest that it is. It is relevant and important, but far from the whole story.
The CFR is easy to calculate. You take the number of people who have died from the disease, and you divide it by the total number of people diagnosed with the disease. So if 10 people have died, and 100 people have been diagnosed with the disease, the CFR is [10 / 100], or 10%.
But it’s important to note that it is the ratio between the number of confirmed deaths from the disease and the number of confirmed cases, not total cases. That means that it is not the same as – and, in fast-moving situations like COVID-19, probably not even very close to – the true risk for an infected person.
Another important metric, which should not be confused with the CFR, is the crude mortality rate.
Crude mortality rate
The “crude mortality rate” is another very simple measure which, like the CFR, gives something that might sound like the answer to the question “if someone is infected, how likely are they to die?”.
But, just as with CFR, it is actually very different.
The crude mortality rate – sometimes also called the crude death rate – measures the share among the entire population that have died from a particular disease. It’s calculated by dividing the number of deaths from the disease by the total population. For instance, if there were 10 deaths in a population of 1,000, the crude mortality rate would be [10 / 1,000], or 1%.
Unfortunately, writers sometimes confuse case fatality rates and crude death rates. A common example is the Spanish flu pandemic in 1918. One estimate for the death toll of the Spanish flu, by Johnson and Mueller (2002), is that the pandemic killed 50 million people. 2 That would have been 2.7% of the world population at the time. This means the crude mortality rate was 2.7%.
But 2.7% is often misreported as the case fatality rate – which is wrong, because not everyone in the world was infected with the virus that caused the Spanish flu. If the crude mortality rate really was 2.7%, then the case fatality rate was much higher – it would be the percentage of people who died after being diagnosed with the disease. [We looked at the global death count of the Spanish flu pandemic and others here.]
Infection fatality rate (IFR)
The key question for understanding the mortality risk of a disease is the following: if someone is infected with the disease how likely is it that they will die from it? The answer to that question is captured by the infection fatality rate, or IFR.
To work out the IFR, we need two numbers: the total number of cases and the total number of deaths from the disease.
The total number of cases is not known, so the IFR cannot be simply calculated from observed data. But, researchers are able to estimate the total number of cases and use that to calculate the IFR – we get to this further below.
Why the Case Fatality Rate does not reflect the risk of dying from COVID-19
There is a straightforward question that most people would like answered. If someone is infected with COVID-19, how likely is that person to die?
This question is simple, but surprisingly hard to answer.
The key point is that the case fatality rate (CFR) – the most commonly discussed measure – is not the answer to the question.
The main reason why it does not answer that question is that the CFR relies on the number of confirmed cases, and many cases are not confirmed.
In order to understand what the case fatality rate can and cannot tell us about a disease outbreak such as COVID-19, it’s important to understand why it is difficult to measure and interpret the numbers.
The case fatality rate isn’t constant: it changes with the context
Sometimes commentators talk about the CFR as if it’s a single, steady number: an unchanging fact about the disease.
But it’s not a biological constant; instead, it reflects the situation in a particular context, at a particular time, in a particular population.
The probability that someone dies from a disease doesn’t just depend on the disease itself, but also on the treatment they receive, and on the patient’s own ability to recover from it.
The CFR of COVID-19 differs by location, and has changed during the early period of the outbreak
The case fatality rate of COVID-19 is not constant. This was clear right from the start of the pandemic. You can see that in the chart below, first published in the Report of the WHO-China Joint Mission on Coronavirus Disease 2019 (COVID-19), in February 2020. 10
It shows the CFR for COVID-19 in several locations in China during the early stages of the outbreak, from the beginning of January to 20th February 2020.
You can see that in the earliest stages of the outbreak the CFR was much higher: 17.3% across China as a whole (in yellow) and greater than 20% in the center of the outbreak, in Wuhan (in blue).
But in the weeks that followed, the CFR declined, reaching as low as 0.7% for patients who first showed symptoms after February 1st. The WHO reported that that was because “the standard of care has evolved over the course of the outbreak”.
You can also see that the CFR was different in different places. By 1st February, the CFR in Wuhan was still 5.8% while it was 0.7% across the rest of China.
This shows that what we said about the CFR generally – that it changes from time to time and place to place – is true for the CFR of COVID-19 specifically. When we talk about the CFR of a disease, we need to talk about it in a specific time and place – the CFR in Wuhan on 23rd February, or in Italy on 4th March – rather than as a single unchanging value.
Case fatality ratio for COVID-19 in China over time and by location, as of 20 February 2020 – Figure 4 in WHO (2020) 11
There are two reasons why the case fatality rate does not reflect the risk of death
If the case fatality rate does not tell us the risk of death for someone infected with the disease, what does it tell us? And how does the CFR compare with the actual mortality risk?
There are two reasons why we would expect the CFR not to represent the real risk. One of them would tend to make the CFR an overestimate – the other would tend to make it an underestimate.
When there are people who have the disease but are not diagnosed, the CFR will overestimate the true risk of death. With COVID-19, we think there are many undiagnosed people.
As we saw above, in our discussion on the difference between total and confirmed cases (here), we do not know the number of total cases. Not everyone is tested for COVID-19, so the total number of cases is higher than the number of confirmed cases.
Whenever there are cases of the disease that are not counted, the probability of dying from the disease is lower than the reported case fatality rate. Remember our imaginary scenario with 10 deaths and 100 cases. The CFR in that example is 10% – but if there actually 500 cases (and we’ve simply missed 400 of them due to lack of testing), then the real risk (the IFR) is just 2%.
Or to summarize in one sentence. If the number of total cases is higher than the number of confirmed cases, then the ratio between deaths and total cases is smaller than the ratio between deaths and confirmed cases. 12
Importantly, this means that the number of tests carried out affects the CFR – you can only confirm a case by testing a patient. So when we compare the CFR between different countries, the differences do not only reflect rates of mortality, but also differences in the scale of testing efforts.
A second consideration is especially important in the early stages of an outbreak: When some people are currently sick and will die of the disease, but have not died yet, the CFR will underestimate the true risk of death.
In ongoing outbreaks, people who are currently sick will eventually die from the disease. This means that they are currently counted as a case, but will only eventually be counted as a death too. With the COVID-19 outbreak, it can take several weeks for people to go from first symptoms to death.
This means that the CFR in the early stages is an underestimate of what it will be when the outbreak has run its course.
Case fatality rate of other diseases
Once again, we should stress what we discussed above. One has to understand the measurement challenges and the definitions to interpret estimates of the CFR for COVID-19, particularly those relating to an ongoing outbreak.
As comparisons, the table shows the case fatality rates for other disease outbreaks. The CFR of SARS-CoV and MERS-CoV were high: 10% and 34%, respectively. 13
The US seasonal flu has a case fatality rate of approximately 0.1% to 0.2%. 14
Sources of data shown in the table:
SARS-CoV: Venkatesh, S. & Memish, Z.A. (2004). SARS: the new challenge to international health and travel medicine. EMHJ – Eastern Mediterranean Health Journal, 10 (4-5), 655-662, 2004.
SARS-CoV and MERS-CoV: Munster, V. J., Koopmans, M., van Doremalen, N., van Riel, D., & de Wit, E. (2020). A novel coronavirus emerging in China—key questions for impact assessment. New England Journal of Medicine, 382(8), 692-694.
Seasonal flu: US Centers for Disease Control and Prevention (CDC). Influenza Burden, 2018-19.
Ebola: Shultz, J. M., Espinel, Z., Espinola, M., & Rechkemmer, A. (2016). Distinguishing epidemiological features of the 2013–2016 West Africa Ebola virus disease outbreak. Disaster Health, 3(3), 78-88.
Ebola: World Health Organization (2020). Ebola virus disease: Factsheet.
| Disease | Estimated case fatality rate (CFR) |
| SARS-CoV | 10% Venkatesh and Memish (2004) Munster et al. (2020) |
| MERS-CoV | 34% Munster et al. (2020) |
| Seasonal flu (US) | 0.1 to 0.2% US CDC |
| Ebola | 50% 40% in the 2013-16 outbreak |
WHO (2020)
Shultz et al. (2016)
Acknowledgements
We would like to acknowledge and thank a number of people in the development of this work: Carl Bergstrom, Bernadeta Dadonaite, Natalie Dean, Joel Hellewell, Jason Hendry, Adam Kucharski, Moritz Kraemer and Eric Topol for their very helpful and detailed comments and suggestions on earlier versions of this work. We thank Tom Chivers for his editorial review and feedback.
And we would like to thank the many hundreds of readers who give us feedback on this work. Your feedback is what allows us to continuously clarify and improve it. We very much appreciate you taking the time to write. We cannot respond to every message we receive, but we do read all feedback and aim to take the many helpful ideas into account.
Endnotes
For examples see Worldometers. Worldometers lists many poor examples of ‘mortality rates’ for COVID-19 without discussion here.
We would therefore calculate the infection fatality rate as:
Infection fatality risk (IFR, in %) = [Number of deaths from disease / total number of cases of disease] x 100
Lipsitch, M., Donnelly, C. A., Fraser, C., Blake, I. M., Cori, A., Dorigatti, I., … & Van Kerkhove, M. D. (2015). Potential biases in estimating absolute and relative case-fatality risks during outbreaks. PLoS Neglected Tropical Diseases, 9(7).
Kobayashi, T., Jung, S. M., Linton, N. M., Kinoshita, R., Hayashi, K., Miyama, T., … & Suzuki, A. (2020). Communicating the Risk of Death from Novel Coronavirus Disease (COVID-19). Journal of Clinical Medicine.
Nishiura, H. (2010). Case fatality ratio of pandemic influenza. The Lancet Infectious Diseases, 10(7), 443.
World Health Organization (2020). Report of the WHO-China Joint Mission on Coronavirus Disease 2019 (COVID-19). Available online at: https://www.who.int/docs/default-source/coronaviruse/who-china-joint-mission-on-covid-19-final-report.pdf
World Health Organization (2020). Report of the WHO-China Joint Mission on Coronavirus Disease 2019 (COVID-19). Available online at: https://www.who.int/docs/default-source/coronaviruse/who-china-joint-mission-on-covid-19-final-report.pdf.
World Health Organization (2020). Report of the WHO-China Joint Mission on Coronavirus Disease 2019 (COVID-19). Available online at: https://www.who.int/docs/default-source/coronaviruse/who-china-joint-mission-on-covid-19-final-report.pdf.
The relationship between CFR and IFR also depends on how large of a discrepancy there is between the number of confirmed and actual deaths, but we’d expect the magnitude of undercounting of deaths to be less than for cases.
Munster, V. J., Koopmans, M., van Doremalen, N., van Riel, D., & de Wit, E. (2020). A novel coronavirus emerging in China—key questions for impact assessment. New England Journal of Medicine, 382(8), 692-694.
The US flu data is sourced from the US CDC. Here we present an upper and lower estimate for the 2018-19 flu season. These two figures reflect whether we look at the percentage of deaths out of the number of symptomatic illnesses (giving us 0.1%), or the number of medical visits (giving us 0.2%). In the traditional calculation of CFR, we would tend to focus on the number of symptomatic illnesses. This is analogous to the number of confirmed cases, on which the COVID-19 figures are based. However, the US CDC derives these figures based on disease outbreak modelling which attempts to account for underreporting – you can read more about how it derives its annual flu figures here.
This means that some of the biases which tend to underestimate the actual number of cases have been corrected for. This is not the case for the COVID-19 figures, so it may be an unfair comparison.
Looking at estimates based on the number of medical visits may discount from the US seasonal flu data many of the kind of mild cases that may have been missed in the COVID-19 confirmed cases. However, this is likely to skew the comparison slightly in the other direction: we know that not all of the confirmed cases included in COVID-19 figures were of a severity such that they would have received a medical visit in the absence of the heightened surveillance of the outbreak.
So, here we present both figures of the US seasonal flu figures: the CFR based on symptomatic illnesses, and those based on medical visits. It’s likely that the fairest comparison to COVID-19 lies somewhere between these two values.
You can find the data for the reported cases, medical visits and deaths from the US Centers for Disease Control and Prevention (CDC) here. The CDC reports 35,520,883 symptomatic cases of influenza in the US and 34,157 deaths from the flu. To calculate the CFR based on symptomatic illnesses, we divide the number of deaths by the number of confirmed cases and find a case fatality rate of 0.1%.(0.1%=[34,157 / 35,520,883] * 100)
Reuse our work freely
All visualizations, data, and code produced by Our World in Data are completely open access under the Creative Commons BY license. You have the permission to use, distribute, and reproduce these in any medium, provided the source and authors are credited.
The data produced by third parties and made available by Our World in Data is subject to the license terms from the original third-party authors. We will always indicate the original source of the data in our documentation, so you should always check the license of any such third-party data before use and redistribution.
Citation
Our articles and data visualizations rely on work from many different people and organizations. When citing this entry, please also cite the underlying data sources. This entry can be cited as: